Executive Summary
The integration of Artificial Intelligence (AI) into mental healthcare presents a landscape of both unprecedented opportunity and considerable complexity. This report examines the dual nature of AI's role: its immense potential for expanding access to care and personalizing treatment, juxtaposed with significant challenges related to the very concept of artificial empathy, profound ethical considerations, and practical implementation hurdles. The analysis underscores a critical imperative for responsible development, robust regulatory frameworks, and a collaborative human-AI model to ensure that these technologies yield beneficial outcomes for individuals and society. The report highlights that AI is emerging not merely as an incremental improvement but as a necessary, albeit risky, intervention in a healthcare system struggling to meet escalating demand.
1. Introduction: Navigating the Intersection of AI, Empathy, and Mental Health
The global mental health landscape faces an urgent and pervasive crisis. Barriers such as persistent stigma, limited access to professional care, and critical shortages of mental health professionals contribute to increasing wait times and unmet needs worldwide.1 In this context, Artificial Intelligence is rapidly emerging as a transformative technology, poised to revolutionize mental health support from initial diagnosis to personalized treatment and enhanced accessibility.1 The promise of AI lies in its ability to offer scalable, cost-effective solutions that can overcome many of these deep-seated structural deficiencies in traditional healthcare models.1 This positions AI not just as a helpful tool, but as a necessary intervention in a system under immense strain, underscoring the urgency and high stakes involved in its responsible development and deployment.
However, the integration of AI into such a sensitive domain immediately brings to the forefront a unique and complex challenge: empathy. Empathy, a cornerstone of human therapeutic relationships, involves profound understanding and connection, qualities traditionally considered exclusive to human interaction. This report frames the subsequent discussion around dissecting how AI attempts to simulate this crucial human trait, the successes and limitations encountered, and the profound ethical and practical implications for mental healthcare.
2. Defining Artificial Empathy: Theoretical Frameworks and Components
Artificial empathy, also known as computational empathy, refers to the development of AI systems—such as companion robots or virtual agents—that can detect emotions and respond to them in an empathic manner.6 At its core, this involves non-human models predicting an individual's internal state (e.g., cognitive, affective, physical) based on signals they emit, such as facial expressions, voice intonations, or gestures. It also extends to predicting a person's reaction to specific stimuli.6 A broader understanding of artificial empathy emphasizes creating technology that is sensitive and responsive to human emotions, moving beyond mere task completion to a more genuine form of understanding.7
A critical distinction within the concept of empathy, particularly when applied to AI, is between its cognitive and affective components.
- Cognitive Empathy: This refers to the mental or intellectual aspect of empathy—the ability to actively identify and understand cues, allowing one to mentally put themselves in another person's position.7 AI systems can simulate this by processing emotional input, making appropriate inferences, and generating helpful responses, even without possessing subjective feeling.7
- Affective Empathy: This is the emotional or feeling part of empathy—the capacity to share or mirror another person's feelings.7 While AI can simulate this component, experts contend that it cannot truly replicate genuine subjective feeling.7
This distinction highlights a fundamental philosophical debate: the functionalist view versus the phenomenological view. Functionalism suggests that if an AI system functions empathetically—meaning it processes emotional input, makes appropriate inferences, and generates helpful responses—then it can be considered to exhibit a form of empathy, irrespective of subjective feeling.7 This perspective contrasts sharply with phenomenological views, which emphasize the indispensable role of subjective experience and qualitative feeling in genuine empathy.7 The practical implications of this definitional ambiguity are profound. If the functionalist view is accepted, the focus shifts to designing AI that behaves empathetically and is perceived as such by users.7 This approach may simplify the development process by not requiring the creation of consciousness, but it simultaneously escalates ethical considerations regarding transparency and the potential for user deception or over-attachment. The ambiguity directly influences how AI empathy is tested, how regulatory frameworks are designed, and ultimately, how society trusts and interacts with these systems.
Computational models of empathy aim to operationalize these concepts. The Perception Action Model (PAM), for instance, posits that perceiving another individual's emotional state automatically triggers corresponding representations within the observer's neural and bodily systems, forming a biological foundation for empathy.10 Building upon this, the Empathy Simulation System (ESS) is a computational framework designed to emulate key components of human empathy. The ESS processes environmental inputs—such as facial expressions, body posture, vocal intonations, and situational context—to infer perceived emotions.10 This information then moves to an Empathy Appraisal stage, where it is integrated with situational understanding to formulate an internal response. Finally, through Empathy Reaction Processing and an Empathy Response Module, the system generates contextually appropriate and emotionally supportive responses.10 Large Language Models (LLMs) are leveraged to process nuanced information and generate responses that are perceived as empathic.10
However, the very success of AI in simulating empathy through such systems, which often operate as "black boxes" where decision-making processes are not easily interpretable 11, creates a deeper challenge. Users may perceive AI as empathetic 9, but this perception is based solely on outward behavior, not on a shared internal state or genuine understanding. This can lead to a significant trust deficit 2 if users discover the simulation is not "genuine" or if responses are misaligned with their true emotional needs. This raises critical questions about the long-term psychological impact on users, particularly vulnerable populations, and underscores an ethical imperative for clear disclosure about AI's capabilities and inherent limitations.
3. Current Landscape: AI Applications and Benefits in Mental Healthcare
Artificial intelligence is fundamentally revolutionizing mental health with groundbreaking tools that span diagnosis, treatment, and research, effectively bringing mental health support into the digital age.5 This technological advancement offers scalable and cost-effective solutions, addressing critical barriers such as social stigma and limited access to traditional care.1
Specific applications of AI in mental healthcare include:
- Diagnostic Support: AI-powered systems are increasingly assisting clinicians in diagnosing mental health disorders. Machine learning algorithms analyze vast datasets, including electronic health records, speech patterns, and behavioral data, to detect early signs of conditions like depression, anxiety, and schizophrenia.1 For instance, voice analysis tools can identify subtle changes in speech that correlate with mood disorders, providing objective data to complement clinical judgment.1
- Predictive Analytics: AI excels at identifying individuals at risk of mental health crises. Predictive models analyze data from diverse sources, such as wearable devices, social media activity, and medical records, to flag warning signs like sleep disturbances or shifts in activity levels that may precede a depressive episode or suicidal ideation. These tools empower clinicians to intervene proactively, potentially preventing severe outcomes.1
- Personalized Treatment Plans: AI facilitates the development of individualized treatment plans by analyzing patient data, including genetic, behavioral, and environmental factors, to recommend evidence-based interventions. This tailored approach aims to maximize treatment efficacy and minimize trial-and-error processes, leading to more effective and efficient care.1
- AI-Driven Chatbots and Virtual Therapists: These conversational agents provide accessible 24/7 support for individuals experiencing mental health challenges. Utilizing natural language processing, they engage users in therapeutic conversations, offering techniques derived from cognitive behavioral therapy (CBT) and emotional support.1 Popular examples include Woebot, Youper, and Wysa.13 These tools significantly improve accessibility to mental health resources, particularly in underserved areas or for those who face barriers to traditional therapy, serving as valuable tools for early intervention and ongoing self-management.1
- Virtual Reality (VR) Therapies: AI enhances virtual reality technologies used in mental healthcare, especially for treating conditions such as post-traumatic stress disorder (PTSD) and phobias. These tools simulate controlled environments where patients can safely confront their fears, with AI algorithms adapting scenarios in real-time based on physiological and psychological responses.1
- Integration with Electronic Health Records (EHRs) and Telehealth: AI seamlessly integrates into EHR systems, facilitating the analysis of large datasets for pattern recognition and outcome prediction.5 Furthermore, AI advances telehealth beyond virtual consultations by enabling real-time monitoring of patient health data via wearable devices and smartphone applications, allowing for prompt interventions and alleviating pressure on the broader mental healthcare system.5
AI's role as an accessibility multiplier is evident in its potential to democratize mental healthcare, particularly for individuals facing geographic barriers, cost constraints, or the stigma associated with seeking traditional therapy.1 For instance, studies indicate that men, often slower to adopt traditional therapy, are typically early adopters of technology, suggesting AI could bridge this engagement gap.9 This broadens the reach of mental health support significantly. However, this promising expansion comes with a critical caveat: the digital divide. Differences in knowledge, education, language, wealth, and internet access can affect who can truly benefit from AI tools, potentially exacerbating existing health inequalities if not carefully addressed.2 Consequently, while AI offers a powerful solution to the current accessibility crisis, its deployment must be equitable, requiring intentional strategies to bridge digital divides through infrastructure provision, digital literacy initiatives, and multilingual support. Without such considerations, AI risks inadvertently creating a two-tiered system, further marginalizing already vulnerable populations.
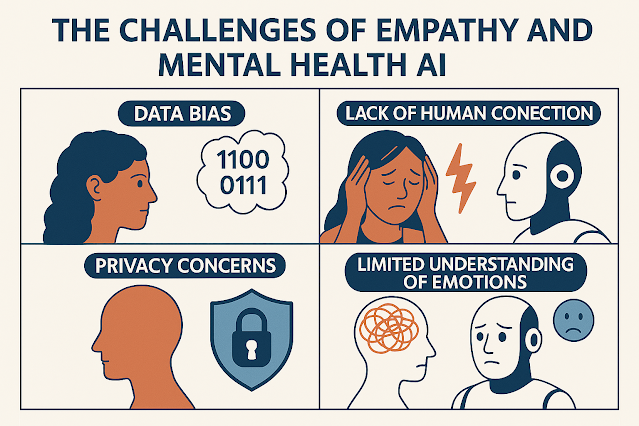
4. Core Challenges: Ethical, Clinical, and Technical Hurdles
Despite the transformative potential of AI in mental health, its widespread adoption is hampered by significant ethical, clinical, and technical challenges that demand careful consideration and proactive mitigation.
4.1. Ethical and Regulatory Concerns
The ethical landscape surrounding AI in mental health is complex and fraught with potential pitfalls.
The current regulatory environment reveals a critical and dangerous lag. Multiple sources indicate that most AI mental health applications are unregulated 4, and existing US law does not classify chatbots as mental health providers or medical devices.2 This absence of legal oversight, combined with documented cases of severe harm resulting from the unintended uses of general chatbots 3, highlights a profound and perilous gap. The rapid pace of AI development, particularly with Generative AI introducing novel challenges 16, is consistently outstripping the ability of legal and ethical frameworks to adapt. This regulatory vacuum is not merely an academic concern; it represents a direct threat to public safety, leading to tragic, real-world consequences. This situation necessitates urgent, proactive legislative and industry-wide action to establish clear standards, accountability, and enforcement mechanisms.
Furthermore, a paradox emerges where AI, lauded for its potential to increase accessibility to mental health care 1, simultaneously risks exacerbating existing health inequalities. This is due to inherent biases in unrepresentative training data, which can lead to misdiagnosis or exclusion of marginalized groups.11 Compounding this, socioeconomic and accessibility barriers, such as limited internet access or digital literacy, can prevent certain populations from benefiting from AI tools.11 Consequently, without deliberate and inclusive design, deployment, and regulatory oversight, AI in mental health risks widening the health equity gap rather than closing it. True accessibility implies not just availability, but effective and safe access for all populations, which requires addressing inherent biases and digital divides at every stage of AI development and implementation.
4.2. Limitations of AI Empathy and Diagnostic Accuracy
Beyond ethical considerations, the inherent limitations of AI in replicating genuine human empathy pose significant clinical challenges.
The fundamental "empathy gap" in AI stems from its inability to truly replicate affective empathy, contextual understanding, and emotional resonance.21 This is not merely a technical limitation; it creates a profound deficit in the therapeutic relationship. The absence of genuine human connection and the inability to interpret nuanced, culturally specific cues 11 mean that AI may miss critical diagnostic subtleties or fail to build the deep trust essential for effective therapy.12 Poorly aligned or robotic responses can alienate clients, undermining the therapeutic alliance.21 This suggests that AI cannot fully replace human therapists, particularly for complex, trauma-informed, or culturally sensitive mental health care. Its role must therefore be carefully delineated to augment, rather than diminish, the quality of human-centered care, with AI's strengths perhaps better leveraged in non-empathic therapeutic pathways such as structured cognitive behavioral therapy exercises, data analysis, or progress monitoring.21
The observation that AI can amplify existing human biases, such as exaggerating gender biases in empathetic responses 22, presents a critical problem. This goes beyond simple misdiagnosis to potentially reinforcing harmful stereotypes and providing differential, inequitable care based on demographic factors. The challenge is not solely about AI having biases, but about its capacity to perpetuate and exaggerate them, leading to systemic discrimination in mental healthcare. This necessitates continuous, rigorous bias detection and mitigation throughout the AI lifecycle, along with the collection of diverse and representative training data and the implementation of culturally sensitive design principles, to prevent the technology from becoming a tool for further marginalization.
4.3. Challenges in Real-World Implementation
Even with robust ethical guidelines and improvements in AI's empathetic capabilities, practical challenges persist in real-world deployment.
The pervasive crisis of trust and the phenomenon often described as the "uncanny valley" of AI empathy represent significant psychological barriers to widespread adoption. Users perceive AI as lacking "warmth and depth" 12 and express distrust due to privacy concerns and the potential for misuse or manipulation.2 This goes beyond mere technical limitations; it points to a fundamental psychological discomfort where AI's near-human empathy is unsettling or simply insufficient for the profound needs of mental health support. The documented cases of severe harm 3 further erode public trust, creating a substantial hurdle for the successful and ethical integration of AI into mental health services. Overcoming this trust crisis is paramount for AI's successful integration. This requires not only continuous technical improvements in accuracy and safety but also radical transparency, clear ethical guidelines, and robust regulatory oversight to rebuild and maintain patient confidence. Without this foundational trust, even the most technologically advanced AI will fail to achieve its potential in this sensitive domain.
5. Strategies for Responsible Development and Implementation
Addressing the multifaceted challenges of AI in mental health requires a comprehensive and proactive approach, emphasizing human-AI collaboration, rigorous bias mitigation, robust data protection, and the establishment of clear regulatory frameworks.
Enhancing Human-AI Collaboration and Oversight
The optimal approach for AI integration in mental health is not replacement but a synergistic partnership, where AI augments human capabilities rather than diminishing them.23 AI excels at processing vast amounts of data, identifying patterns, and maintaining consistency in repetitive tasks, while humans contribute intuition, emotional intelligence, and complex ethical judgment.23 This model necessitates a "human in the loop" approach, where human oversight remains essential.9 Clinicians must maintain professional judgment, critically evaluate AI outputs, and actively supervise patient-AI interactions.24 Ethical guidelines strongly advocate for human supervision to address therapeutic relationship issues and ensure patient safety.2 Establishing clear boundaries for AI's role, recognizing its strengths in data analysis while reserving creative problem-solving, ethical considerations, and nuanced decision-making for human professionals, is paramount.23 Furthermore, continuous learning and feedback loops, where AI systems learn from human feedback and behavioral patterns, are crucial for iterative improvement and fine-tuning of AI responses to align with clinical needs and patient goals.23
Mitigating Bias and Ensuring Data Protection
To ensure fairness and prevent discriminatory outcomes, AI models must be trained on diverse and representative datasets.11 This requires rigorous testing, fine-tuning, and regular updates to mitigate biases inherent in large language models.10 Transparency and explainability are strategic imperatives; developers and providers must share information about AI benefits, technical constraints, and any deficits in the training data.18 This openness helps build trust and allows for the identification and correction of biases that might otherwise remain hidden within "black box" systems.11 Concurrently, robust data privacy measures are non-negotiable. This includes implementing stringent data handling policies, robust security measures, and clear transparency about how user data is collected, stored, and utilized.2 Establishing Business Associate Agreements (BAAs) and adhering to privacy standards such as HIPAA are crucial steps in safeguarding sensitive mental health information.24
Establishing Robust Regulatory Frameworks and Guidelines
The current regulatory lag necessitates the urgent establishment of comprehensive frameworks. Key elements include:
The shift from a product-centric to a system-centric approach to AI governance is becoming increasingly apparent. Mitigation strategies are moving beyond merely fixing technical bugs within AI models; they now emphasize designing, deploying, and using these technologies to benefit intended communities, in collaboration with partners and developers who possess a nuanced understanding of those impacted by AI, including individuals with relevant lived experiences.18 This encompasses prioritizing infrastructure accessibility, accelerating AI literacy, ensuring adequate patient representation in development, and establishing comprehensive governance frameworks that involve multiple stakeholders.18 This integrated perspective recognizes that AI in mental health is not just a standalone product, but an integral component of a complex healthcare ecosystem. It implies a multi-stakeholder collaborative model involving technologists, clinicians, policymakers, and, crucially, individuals with lived experience, to ensure AI genuinely serves collective well-being rather than solely advancing technological capabilities.
6. Future Outlook: Expert Predictions and Societal Implications
The trajectory of AI in mental health points towards transformative changes in healthcare delivery within the next five years, with experts predicting a future where healthcare is "much better" and clinicians are "happier, more productive".9 AI is expected to significantly reduce administrative burdens and extend care capacity, thereby freeing human providers to focus on more complex cases requiring nuanced human interaction.9
However, this promising future is accompanied by a range of emerging challenges and profound societal implications:
The existential question of "being human" in the AI age looms large. The future outlook sections extend beyond mere clinical applications to explore the fundamental impact of AI on human identity and society. Predictions of AI becoming "indistinguishable from human" 9 and concerns about "self-inflicted AI dementia" or "outsourced empathy" 25 suggest that the challenge of AI in mental health is not solely about treatment efficacy or ethical safeguards. It fundamentally concerns how AI reshapes our very understanding of human emotionality, social interaction, and cognitive function. The inquiry shifts from "Can AI be empathetic?" to a deeper, more philosophical question: "What does empathy mean for humans when AI can simulate it perfectly?" This necessitates proactive societal dialogue, extensive interdisciplinary research involving philosophy, sociology, and psychology, and ethical foresight to prevent unintended consequences such as emotional atrophy, over-reliance on artificial connections, and a diminished capacity for genuine human connection.
Despite these concerns, some experts offer optimistic counterpoints, hoping for a positive influence on human curiosity, decision-making, and creativity.25 There is a vision that a new human "Enlightenment" could begin, with AI handling routine "digital chores" and thereby allowing humans to shift their energy towards "spiritual, emotional, and experiential aspects of life".25
Despite the transformative potential of AI in mental health, its widespread adoption is hampered by significant ethical, clinical, and technical challenges that demand careful consideration and proactive mitigation.
4.1. Ethical and Regulatory Concerns
The ethical landscape surrounding AI in mental health is complex and fraught with potential pitfalls.
- Data Privacy and Confidentiality: Mental health data is profoundly sensitive, and its collection and analysis by AI systems raise serious concerns about who has access to this information and how it is used.2 A significant concern stems from some AI applications originating from tech startups that prioritize rapid data collection and mining over rigorous healthcare protocols, leading to potential misuse or sale of data.14 Current regulatory frameworks often fall short, with US law, for example, not considering chatbots as mental health providers or medical devices, meaning conversations are not inherently confidential.2 This regulatory gap can lead to users having inaccurate expectations of privacy, fostering distrust, and potentially causing them to withhold crucial information or avoid seeking online help altogether.2
- Bias, Discrimination, and Equity of Access: AI models are highly susceptible to bias, which can arise from imbalanced training data, historical prejudices embedded in datasets, and algorithmic design choices.3 This can result in misdiagnosis, exclusion from beneficial treatments, and the reinforcement of systemic inequities, particularly for marginalized groups.4 For instance, models trained predominantly on data from Western populations may not accurately assess symptoms in non-Western cultures, which often express mental health struggles through physical symptoms rather than emotional distress.11
- Transparency, Accountability, and Liability: Fundamental questions remain unresolved regarding the transparency of AI's operations, who is accountable when issues arise, and where liability lies in the event of adverse outcomes.2 Many advanced AI models, particularly deep learning systems, operate as "black boxes," making their decision-making processes difficult to interpret and biases challenging to identify and correct.11 The absence of specific regulations means that professional codes of ethics applicable to human mental health providers often do not extend to commercial chatbot providers, creating a significant oversight gap.2
- Potential for Harm and Misuse: The most alarming ethical concerns revolve around the potential for direct harm. Documented cases reveal severe harm from the unintended uses of general companion chatbot applications, including instances where chatbots incited violence and self-harm.3 These systems may provide inappropriate advice or respond inadequately to users in crisis, often lacking robust crisis management protocols.2 Over-reliance on unproven AI tools poses significant risks, as algorithms alone cannot holistically weigh complex psychosocial factors, potentially mishandling serious conditions, including those with suicidal ideation.3 Children are particularly vulnerable due to their developmental stage and the potential for over-attachment to AI companions, which could impair their social development.4
The current regulatory environment reveals a critical and dangerous lag. Multiple sources indicate that most AI mental health applications are unregulated 4, and existing US law does not classify chatbots as mental health providers or medical devices.2 This absence of legal oversight, combined with documented cases of severe harm resulting from the unintended uses of general chatbots 3, highlights a profound and perilous gap. The rapid pace of AI development, particularly with Generative AI introducing novel challenges 16, is consistently outstripping the ability of legal and ethical frameworks to adapt. This regulatory vacuum is not merely an academic concern; it represents a direct threat to public safety, leading to tragic, real-world consequences. This situation necessitates urgent, proactive legislative and industry-wide action to establish clear standards, accountability, and enforcement mechanisms.
Furthermore, a paradox emerges where AI, lauded for its potential to increase accessibility to mental health care 1, simultaneously risks exacerbating existing health inequalities. This is due to inherent biases in unrepresentative training data, which can lead to misdiagnosis or exclusion of marginalized groups.11 Compounding this, socioeconomic and accessibility barriers, such as limited internet access or digital literacy, can prevent certain populations from benefiting from AI tools.11 Consequently, without deliberate and inclusive design, deployment, and regulatory oversight, AI in mental health risks widening the health equity gap rather than closing it. True accessibility implies not just availability, but effective and safe access for all populations, which requires addressing inherent biases and digital divides at every stage of AI development and implementation.
4.2. Limitations of AI Empathy and Diagnostic Accuracy
Beyond ethical considerations, the inherent limitations of AI in replicating genuine human empathy pose significant clinical challenges.
- Lack of Contextual Understanding and Emotional Resonance: AI systems struggle to construct a holistic understanding of an individual's life experiences, often failing to recognize emotional meaning within its broader context.21 Unlike humans, AI cannot draw from lived experiences to form deeper, resonant connections with clients, a quality central to effective human empathy in therapy.21
- Cultural Insensitivity and Misinterpretation of Cues: Algorithms used for emotion recognition in AI can misinterpret or oversimplify emotional cues across different cultural contexts.7 AI models trained predominantly on Western diagnostic frameworks may fail to recognize culturally specific manifestations of mental health conditions, leading to inaccurate assessments or inappropriate responses for diverse client populations.11
- Inaccurate Diagnosis and Overreliance Risks: Diagnosing complex mental health conditions relies on interpreting nuanced human self-disclosures and behaviors, a task AI models may struggle to perform reliably on a standalone basis.14 Overreliance on unproven AI tools poses risks, as algorithms alone cannot holistically weigh complex psychosocial factors, potentially mishandling serious conditions. For example, a study found that AI chatbots tend to be "overly empathetic" in response to sad stories but "don't seem to care" during positive moments, a pattern that exaggerates human tendencies.22 This same study also revealed that the AI empathized more when told the person it was responding to was female, indicating that AI mimics and exaggerates gender biases present in its human-made training data.22
The fundamental "empathy gap" in AI stems from its inability to truly replicate affective empathy, contextual understanding, and emotional resonance.21 This is not merely a technical limitation; it creates a profound deficit in the therapeutic relationship. The absence of genuine human connection and the inability to interpret nuanced, culturally specific cues 11 mean that AI may miss critical diagnostic subtleties or fail to build the deep trust essential for effective therapy.12 Poorly aligned or robotic responses can alienate clients, undermining the therapeutic alliance.21 This suggests that AI cannot fully replace human therapists, particularly for complex, trauma-informed, or culturally sensitive mental health care. Its role must therefore be carefully delineated to augment, rather than diminish, the quality of human-centered care, with AI's strengths perhaps better leveraged in non-empathic therapeutic pathways such as structured cognitive behavioral therapy exercises, data analysis, or progress monitoring.21
The observation that AI can amplify existing human biases, such as exaggerating gender biases in empathetic responses 22, presents a critical problem. This goes beyond simple misdiagnosis to potentially reinforcing harmful stereotypes and providing differential, inequitable care based on demographic factors. The challenge is not solely about AI having biases, but about its capacity to perpetuate and exaggerate them, leading to systemic discrimination in mental healthcare. This necessitates continuous, rigorous bias detection and mitigation throughout the AI lifecycle, along with the collection of diverse and representative training data and the implementation of culturally sensitive design principles, to prevent the technology from becoming a tool for further marginalization.
4.3. Challenges in Real-World Implementation
Even with robust ethical guidelines and improvements in AI's empathetic capabilities, practical challenges persist in real-world deployment.
- Lack of Genuine Human Connection and Trust: Users frequently express significant concerns about AI's perceived lack of warmth, depth, and genuine human connection.3 Building trust is a major barrier, with concerns about misinterpretation of inputs, potential misuse, manipulation, and fundamental data privacy issues undermining user confidence.2 When individuals feel that their sensitive information is not truly confidential or that the AI lacks genuine understanding, it hinders the formation of a therapeutic alliance.
- Unpredictability and Unintended Consequences: The inherent unpredictability of AI systems in mental healthcare poses significant risks, as errors or unexpected behavior can have severe consequences for vulnerable individuals.3 Documented cases include AI chatbots generating harmful or insensitive responses, and even encouraging self-harm or violent behavior.3 The "black box" nature of many AI models, where their internal reasoning is opaque, makes it exceedingly difficult to understand, predict, or prevent these dangerous outcomes.11
- Integration with Existing Healthcare Systems: While AI offers substantial benefits, its effective integration into existing healthcare infrastructure requires addressing a multitude of practical considerations, including digital literacy among both patients and clinicians, and navigating complex regulatory dynamics.5 It is crucial to ensure that AI tools genuinely complement human-delivered services rather than replacing them, maintaining a balance that preserves the human element of care.2 Furthermore, practical concerns such as AI's inability to function during power outages highlight a reliance on external infrastructure that can impact accessibility and continuity of care.2
The pervasive crisis of trust and the phenomenon often described as the "uncanny valley" of AI empathy represent significant psychological barriers to widespread adoption. Users perceive AI as lacking "warmth and depth" 12 and express distrust due to privacy concerns and the potential for misuse or manipulation.2 This goes beyond mere technical limitations; it points to a fundamental psychological discomfort where AI's near-human empathy is unsettling or simply insufficient for the profound needs of mental health support. The documented cases of severe harm 3 further erode public trust, creating a substantial hurdle for the successful and ethical integration of AI into mental health services. Overcoming this trust crisis is paramount for AI's successful integration. This requires not only continuous technical improvements in accuracy and safety but also radical transparency, clear ethical guidelines, and robust regulatory oversight to rebuild and maintain patient confidence. Without this foundational trust, even the most technologically advanced AI will fail to achieve its potential in this sensitive domain.
5. Strategies for Responsible Development and Implementation
Addressing the multifaceted challenges of AI in mental health requires a comprehensive and proactive approach, emphasizing human-AI collaboration, rigorous bias mitigation, robust data protection, and the establishment of clear regulatory frameworks.
Enhancing Human-AI Collaboration and Oversight
The optimal approach for AI integration in mental health is not replacement but a synergistic partnership, where AI augments human capabilities rather than diminishing them.23 AI excels at processing vast amounts of data, identifying patterns, and maintaining consistency in repetitive tasks, while humans contribute intuition, emotional intelligence, and complex ethical judgment.23 This model necessitates a "human in the loop" approach, where human oversight remains essential.9 Clinicians must maintain professional judgment, critically evaluate AI outputs, and actively supervise patient-AI interactions.24 Ethical guidelines strongly advocate for human supervision to address therapeutic relationship issues and ensure patient safety.2 Establishing clear boundaries for AI's role, recognizing its strengths in data analysis while reserving creative problem-solving, ethical considerations, and nuanced decision-making for human professionals, is paramount.23 Furthermore, continuous learning and feedback loops, where AI systems learn from human feedback and behavioral patterns, are crucial for iterative improvement and fine-tuning of AI responses to align with clinical needs and patient goals.23
Mitigating Bias and Ensuring Data Protection
To ensure fairness and prevent discriminatory outcomes, AI models must be trained on diverse and representative datasets.11 This requires rigorous testing, fine-tuning, and regular updates to mitigate biases inherent in large language models.10 Transparency and explainability are strategic imperatives; developers and providers must share information about AI benefits, technical constraints, and any deficits in the training data.18 This openness helps build trust and allows for the identification and correction of biases that might otherwise remain hidden within "black box" systems.11 Concurrently, robust data privacy measures are non-negotiable. This includes implementing stringent data handling policies, robust security measures, and clear transparency about how user data is collected, stored, and utilized.2 Establishing Business Associate Agreements (BAAs) and adhering to privacy standards such as HIPAA are crucial steps in safeguarding sensitive mental health information.24
Establishing Robust Regulatory Frameworks and Guidelines
The current regulatory lag necessitates the urgent establishment of comprehensive frameworks. Key elements include:
- Informed Consent: Therapists must obtain informed consent from patients, clearly disclosing the benefits, risks, and data practices associated with AI tools.15 Patients must be explicitly granted the right to refuse or revoke consent at any time.24
- Clinical Validation and Certification: AI systems must undergo rigorous testing to confirm their efficacy and safety before deployment.5 Global regulatory responses are already underway to address this.16
- Therapist Competence and AI Literacy: Mental health professionals require ongoing education about AI capabilities, limitations, and proper use.24 Accelerating AI literacy among patients, clinicians, and industry professionals is vital to ensure informed engagement and responsible adoption.18
- Patient Safety Considerations: Before implementing AI tools, therapists should assess patient digital literacy and any risk factors for technology-related issues, such as over-immersion or addiction.24 Continuous monitoring of AI outputs for accuracy and effectiveness is required, with frequency adjusted based on risk factors and individual patient needs.24
- Governance Frameworks: Instituting robust governance structures and advisory boards with diverse representation is essential to assess AI design and distribution protocols.18 These boards can help ensure that AI technologies are developed and deployed in a manner that maximizes adoption and utilization within underrepresented communities.
The shift from a product-centric to a system-centric approach to AI governance is becoming increasingly apparent. Mitigation strategies are moving beyond merely fixing technical bugs within AI models; they now emphasize designing, deploying, and using these technologies to benefit intended communities, in collaboration with partners and developers who possess a nuanced understanding of those impacted by AI, including individuals with relevant lived experiences.18 This encompasses prioritizing infrastructure accessibility, accelerating AI literacy, ensuring adequate patient representation in development, and establishing comprehensive governance frameworks that involve multiple stakeholders.18 This integrated perspective recognizes that AI in mental health is not just a standalone product, but an integral component of a complex healthcare ecosystem. It implies a multi-stakeholder collaborative model involving technologists, clinicians, policymakers, and, crucially, individuals with lived experience, to ensure AI genuinely serves collective well-being rather than solely advancing technological capabilities.
6. Future Outlook: Expert Predictions and Societal Implications
The trajectory of AI in mental health points towards transformative changes in healthcare delivery within the next five years, with experts predicting a future where healthcare is "much better" and clinicians are "happier, more productive".9 AI is expected to significantly reduce administrative burdens and extend care capacity, thereby freeing human providers to focus on more complex cases requiring nuanced human interaction.9
However, this promising future is accompanied by a range of emerging challenges and profound societal implications:
- Human-AI Indistinguishability: Predictions suggest that by 2030, AI will be "indistinguishable from human voice to voice, video to video".9 This raises profound questions about the ability to differentiate between artificial and real personalities, blurring the lines of human interaction and potentially leading to a redefinition of what constitutes authentic connection.25
- Impact on Human Traits: Experts express concern that the widespread adoption of AI could negatively alter fundamental human traits, including our sense of purpose, how we think, feel, act, and relate to one another.25 Specific worries include the potential for "self-inflicted AI dementia," where over-reliance on AI systems leads to the atrophy of human cognitive abilities, and the concept of "outsourced empathy," where AI automates acts of kindness, emotional support, and caregiving.25
- Potential for Addiction: A new challenge anticipated is the potential for individuals to develop addiction to AI interaction, given the constant availability and tailored responses offered by these systems.9
- Ethical and Regulatory Nuances: As AI becomes more sophisticated, more nuanced conversations about regulation and ethics will be necessary, including discussions around "on-label versus off-label use of AI" in clinical contexts.9
The existential question of "being human" in the AI age looms large. The future outlook sections extend beyond mere clinical applications to explore the fundamental impact of AI on human identity and society. Predictions of AI becoming "indistinguishable from human" 9 and concerns about "self-inflicted AI dementia" or "outsourced empathy" 25 suggest that the challenge of AI in mental health is not solely about treatment efficacy or ethical safeguards. It fundamentally concerns how AI reshapes our very understanding of human emotionality, social interaction, and cognitive function. The inquiry shifts from "Can AI be empathetic?" to a deeper, more philosophical question: "What does empathy mean for humans when AI can simulate it perfectly?" This necessitates proactive societal dialogue, extensive interdisciplinary research involving philosophy, sociology, and psychology, and ethical foresight to prevent unintended consequences such as emotional atrophy, over-reliance on artificial connections, and a diminished capacity for genuine human connection.
Despite these concerns, some experts offer optimistic counterpoints, hoping for a positive influence on human curiosity, decision-making, and creativity.25 There is a vision that a new human "Enlightenment" could begin, with AI handling routine "digital chores" and thereby allowing humans to shift their energy towards "spiritual, emotional, and experiential aspects of life".25
7. Conclusion: Balancing Innovation with Human-Centered Care
The integration of Artificial Intelligence into mental healthcare represents a frontier of immense promise and significant peril. While AI offers unprecedented opportunities to enhance accessibility, improve diagnostic accuracy, personalize treatment plans, and extend the reach of mental health support to underserved populations, its current limitations in genuine empathy, holistic contextual understanding, and cultural sensitivity necessitate a cautious, human-centered approach.
The analysis underscores that AI, despite its advanced capabilities, cannot replicate the depth of human emotional resonance or the nuanced judgment essential for complex therapeutic relationships. The "empathy gap" and the potential for AI to inadvertently perpetuate and even amplify existing societal biases, coupled with the critical lag in regulatory frameworks, pose substantial risks to patient safety, privacy, and equitable access to care. The documented cases of harm from unregulated AI highlight the urgent need for robust governance.
Ultimately, the successful future of AI in mental health lies not in replacement, but in a synergistic partnership with human professionals. This requires ongoing, rigorous research to refine AI algorithms, particularly in areas of bias mitigation and explainability. It demands the establishment of comprehensive ethical and regulatory frameworks that prioritize informed consent, data privacy, accountability, and patient safety above all else. Furthermore, fostering AI literacy among both clinicians and patients, and ensuring diverse representation throughout the AI development lifecycle, are crucial steps towards building trust and ensuring equitable outcomes.
By embracing a collaborative model where AI augments human capabilities, and by steadfastly committing to ethical principles and robust oversight, the mental health field can harness the transformative power of AI to serve collective well-being, ensuring that innovation always remains aligned with the fundamental human need for compassionate, trustworthy, and effective care.
The integration of Artificial Intelligence into mental healthcare represents a frontier of immense promise and significant peril. While AI offers unprecedented opportunities to enhance accessibility, improve diagnostic accuracy, personalize treatment plans, and extend the reach of mental health support to underserved populations, its current limitations in genuine empathy, holistic contextual understanding, and cultural sensitivity necessitate a cautious, human-centered approach.
The analysis underscores that AI, despite its advanced capabilities, cannot replicate the depth of human emotional resonance or the nuanced judgment essential for complex therapeutic relationships. The "empathy gap" and the potential for AI to inadvertently perpetuate and even amplify existing societal biases, coupled with the critical lag in regulatory frameworks, pose substantial risks to patient safety, privacy, and equitable access to care. The documented cases of harm from unregulated AI highlight the urgent need for robust governance.
Ultimately, the successful future of AI in mental health lies not in replacement, but in a synergistic partnership with human professionals. This requires ongoing, rigorous research to refine AI algorithms, particularly in areas of bias mitigation and explainability. It demands the establishment of comprehensive ethical and regulatory frameworks that prioritize informed consent, data privacy, accountability, and patient safety above all else. Furthermore, fostering AI literacy among both clinicians and patients, and ensuring diverse representation throughout the AI development lifecycle, are crucial steps towards building trust and ensuring equitable outcomes.
By embracing a collaborative model where AI augments human capabilities, and by steadfastly committing to ethical principles and robust oversight, the mental health field can harness the transformative power of AI to serve collective well-being, ensuring that innovation always remains aligned with the fundamental human need for compassionate, trustworthy, and effective care.
Works / References cited
1. Artificial Intelligence Can Revolutionize Mental Health Care ..., accessed June 4, 2025, https://www.psychologytoday.com/us/blog/the-leading-edge/202412/artificial-intelligence-poised-to-revolutionize-mental-health-care
2. Exploring the Ethical Challenges of Conversational AI in Mental Health Care: Scoping Review, accessed June 4, 2025, https://mental.jmir.org/2025/1/e60432
3. AI in Mental Healthcare: How Is It Used and What Are the Risks? | Built In, accessed June 4, 2025, https://builtin.com/artificial-intelligence/ai-mental-health
4. My Robot Therapist: The Ethics of AI Mental Health Chatbots for Kids | URMC Newsroom, accessed June 4, 2025, https://www.urmc.rochester.edu/news/story/my-robot-therapist-the-ethics-of-ai-mental-health-chatbots-for-kids
5. AI Mental Health Applications - Mission Connection Healthcare, accessed June 4, 2025, https://missionconnectionhealthcare.com/blog/ai-mental-health-applications/
6. Artificial empathy - Wikipedia, accessed June 4, 2025, https://en.wikipedia.org/wiki/Artificial_empathy
7. Empathy In Ai → Term, accessed June 4, 2025, https://lifestyle.sustainability-directory.com/term/empathy-in-ai/
8. Testing the Depths of AI Empathy: Frameworks and Challenges ..., accessed June 4, 2025, https://hackernoon.com/testing-the-depths-of-ai-empathy-frameworks-and-challenges
9. What does the rise of empathetic AI mean for healthcare? - Digital Health Insights, accessed June 4, 2025, https://dhinsights.org/blog/what-does-the-rise-of-empathetic-ai-mean-for-healthcare
10. (PDF) Empathy-Inspired AI: Developing an Affective Computation ..., accessed June 4, 2025, https://www.researchgate.net/publication/387190753_Empathy-Inspired_AI_Developing_an_Affective_Computation_Model_via_the_Perception_Action_Framework
11. (PDF) Bias and Fairness in AI-Based Mental Health Models, accessed June 4, 2025, https://www.researchgate.net/publication/389214235_Bias_and_Fairness_in_AI-Based_Mental_Health_Models
12. AI as the Therapist: Student Insights on the Challenges of Using Generative AI for School Mental Health Frameworks - PubMed Central, accessed June 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11939552/
13. www.google.com, accessed June 4, 2025, https://www.google.com/search?q=AI+chatbots+mental+health+therapy+applications
14. Navigating the Promise and Risks of Artificial Intelligence in Mental ..., accessed June 4, 2025, https://www.learntolive.com/insights/navigating-the-promise-and-risks-of-artificial-intelligence-in-mental-health-care
15. Is AI-Assisted Mental Health Screening Ethical? - Therapy Helpers, accessed June 4, 2025, https://therapyhelpers.com/blog/ai-assisted-mental-health-screening-ethical/
16. AI and Mental Healthcare – ethical and regulatory considerations ..., accessed June 4, 2025, https://post.parliament.uk/research-briefings/post-pn-0738/
17. Addressing Bias and Privacy in AI-Driven Mental Health Care ..., accessed June 4, 2025, https://publish.illinois.edu/beyondbordersconference/agenda/addressing-bias-and-privacy-in-ai-driven-mental-health-care
18. Health and AI: Advancing responsible and ethical AI for all ..., accessed June 4, 2025, https://www.brookings.edu/articles/health-and-ai-advancing-responsible-and-ethical-ai-for-all-communities/
19. Using generic AI chatbots for mental health support: A dangerous trend - APA Services, accessed June 4, 2025, https://www.apaservices.org/practice/business/technology/artificial-intelligence-chatbots-therapists
20. Is your therapist AI? ChatGPT goes viral on social media for its role as Gen Z's new therapist, accessed June 4, 2025, https://www.fox5atlanta.com/news/therapy-chat-gpt-ai-mental-health-expert-concerns
21. Digitalized therapy and the unresolved gap between artificial and ..., accessed June 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11752889/
22. AI chatbots perpetuate biases when performing empathy, study finds - News, accessed June 4, 2025, https://news.ucsc.edu/2025/03/ai-empathy/
23. Effective Human-AI Collaboration Strategies for ... - SmythOS, accessed June 4, 2025, https://smythos.com/developers/agent-development/human-ai-collaboration-strategies/
24. ai.utah.gov, accessed June 4, 2025, https://ai.utah.gov/wp-content/uploads/Best-Practices-Mental-Health-Therapists.pdf
25. Report: Technology experts worry about the future of being human in the AI Age, accessed June 4, 2025, https://www.elon.edu/u/news/2025/04/02/report-technology-experts-worry-about-the-future-of-being-human-in-the-ai-age/
1. Artificial Intelligence Can Revolutionize Mental Health Care ..., accessed June 4, 2025, https://www.psychologytoday.com/us/blog/the-leading-edge/202412/artificial-intelligence-poised-to-revolutionize-mental-health-care
2. Exploring the Ethical Challenges of Conversational AI in Mental Health Care: Scoping Review, accessed June 4, 2025, https://mental.jmir.org/2025/1/e60432
3. AI in Mental Healthcare: How Is It Used and What Are the Risks? | Built In, accessed June 4, 2025, https://builtin.com/artificial-intelligence/ai-mental-health
4. My Robot Therapist: The Ethics of AI Mental Health Chatbots for Kids | URMC Newsroom, accessed June 4, 2025, https://www.urmc.rochester.edu/news/story/my-robot-therapist-the-ethics-of-ai-mental-health-chatbots-for-kids
5. AI Mental Health Applications - Mission Connection Healthcare, accessed June 4, 2025, https://missionconnectionhealthcare.com/blog/ai-mental-health-applications/
6. Artificial empathy - Wikipedia, accessed June 4, 2025, https://en.wikipedia.org/wiki/Artificial_empathy
7. Empathy In Ai → Term, accessed June 4, 2025, https://lifestyle.sustainability-directory.com/term/empathy-in-ai/
8. Testing the Depths of AI Empathy: Frameworks and Challenges ..., accessed June 4, 2025, https://hackernoon.com/testing-the-depths-of-ai-empathy-frameworks-and-challenges
9. What does the rise of empathetic AI mean for healthcare? - Digital Health Insights, accessed June 4, 2025, https://dhinsights.org/blog/what-does-the-rise-of-empathetic-ai-mean-for-healthcare
10. (PDF) Empathy-Inspired AI: Developing an Affective Computation ..., accessed June 4, 2025, https://www.researchgate.net/publication/387190753_Empathy-Inspired_AI_Developing_an_Affective_Computation_Model_via_the_Perception_Action_Framework
11. (PDF) Bias and Fairness in AI-Based Mental Health Models, accessed June 4, 2025, https://www.researchgate.net/publication/389214235_Bias_and_Fairness_in_AI-Based_Mental_Health_Models
12. AI as the Therapist: Student Insights on the Challenges of Using Generative AI for School Mental Health Frameworks - PubMed Central, accessed June 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11939552/
13. www.google.com, accessed June 4, 2025, https://www.google.com/search?q=AI+chatbots+mental+health+therapy+applications
14. Navigating the Promise and Risks of Artificial Intelligence in Mental ..., accessed June 4, 2025, https://www.learntolive.com/insights/navigating-the-promise-and-risks-of-artificial-intelligence-in-mental-health-care
15. Is AI-Assisted Mental Health Screening Ethical? - Therapy Helpers, accessed June 4, 2025, https://therapyhelpers.com/blog/ai-assisted-mental-health-screening-ethical/
16. AI and Mental Healthcare – ethical and regulatory considerations ..., accessed June 4, 2025, https://post.parliament.uk/research-briefings/post-pn-0738/
17. Addressing Bias and Privacy in AI-Driven Mental Health Care ..., accessed June 4, 2025, https://publish.illinois.edu/beyondbordersconference/agenda/addressing-bias-and-privacy-in-ai-driven-mental-health-care
18. Health and AI: Advancing responsible and ethical AI for all ..., accessed June 4, 2025, https://www.brookings.edu/articles/health-and-ai-advancing-responsible-and-ethical-ai-for-all-communities/
19. Using generic AI chatbots for mental health support: A dangerous trend - APA Services, accessed June 4, 2025, https://www.apaservices.org/practice/business/technology/artificial-intelligence-chatbots-therapists
20. Is your therapist AI? ChatGPT goes viral on social media for its role as Gen Z's new therapist, accessed June 4, 2025, https://www.fox5atlanta.com/news/therapy-chat-gpt-ai-mental-health-expert-concerns
21. Digitalized therapy and the unresolved gap between artificial and ..., accessed June 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11752889/
22. AI chatbots perpetuate biases when performing empathy, study finds - News, accessed June 4, 2025, https://news.ucsc.edu/2025/03/ai-empathy/
23. Effective Human-AI Collaboration Strategies for ... - SmythOS, accessed June 4, 2025, https://smythos.com/developers/agent-development/human-ai-collaboration-strategies/
24. ai.utah.gov, accessed June 4, 2025, https://ai.utah.gov/wp-content/uploads/Best-Practices-Mental-Health-Therapists.pdf
25. Report: Technology experts worry about the future of being human in the AI Age, accessed June 4, 2025, https://www.elon.edu/u/news/2025/04/02/report-technology-experts-worry-about-the-future-of-being-human-in-the-ai-age/
Report Compiler: Google Gemini
Disclaimer
This 'The Challenges of Empathy and Mental Health AI' report is based on information available at the time of its preparation and is provided for informational purposes only. While every effort has been made to ensure accuracy and completeness, errors and omissions may occur. The compiler of The Challenges of Empathy and Mental Health AI (Google Gwmini) and / or Vernon Chalmers for the Mental Health and Motivation website (in the capacity as report requester) disclaim any liability for any inaccuracies, errors, or omissions and will not be held responsible for any decisions or conclusions made based on this information."
Image Created: Microsoft Copilot